- Home
- About Us
- Meet Our Team
- Facilities
- Services
- Expertise
- Anterior Lamellar Transplants
- Artificial Cornea
- Cataract Surgery In Children
- Complex Cataract Surgeries
- Corneal Infections
- Corneal Transplants In Children
- Dry Eye Disorders
- Keratoconus
- Lasik And Refractive Surgery
- Ocular Allergies
- Ocular Inflammation
- Ocular Surface Reconstruction
- Pterygium Management
- Secondary Iol Implants
- Sutureless Corneal Transplants
- Patient Information
- Academics
- Darshan Activites
- Contact us
ANTERIOR LAMELLAR TRANSPLANTS
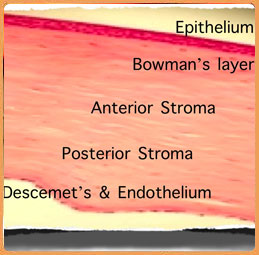
The cornea has a layered structure and is composed of the epithelium with its basement membrane on the top, and the endothelium with the Descemet’s membrane on the bottom. The rest of the corneal stroma – which is present between these 2 layers – constitutes 90% of the corneal thickness and is composed of sheets of collagen arranged in a precise manner.
The principal function of the cornea is to transmit visible light into the eye. By virtue of its regular curvature, it also assists in focusing the incoming rays of light, such that they reach the retina in a coordinated manner. Many diseases can affect these functions of the cornea.
Corneal scars, either from injury or surgery, result in disorganization of the collagen layers in the stroma, and this prevents the transmission of light into the eye. Sometimes, such a loss of corneal clarity can also be due to genetic diseases (dystrophies), or other causes (degenerations).
Sometimes, a clear cornea may be thin and irregular in shape, and while it still transmits light, it no longer focuses it precisely on the retina. The most common cause for such a condition is keratoconus, a genetic condition, but rarely this may also result from extreme corneal weakness after LASIK surgery.
Traditionally, such conditions are treated by a full-thickness corneal replacement procedure termed penetrating keratoplasty (PK). Although effective, the risk of corneal rejection exists. With recent advances in technique, a lamellar procedure is the preferred approach in such eyes. In this surgery, the corneal endothelium and Descemet’s membrane in the host are retained and only the anterior 95% of the corneal stroma is replaced. This provides extremely good results without fear of corneal graft rejection – a tremendous advantage for the patient. The use of the “Big Bubble” technique has greatly increased the success rate of this procedure.
In moderate disease, the newer option of collagen cross-linking (C3R) to stiffen the cornea, can slow or arrest disease progression. Dr Srinivas K Rao is a pioneer in this technique with more than 400 cases done thus far. A recent advance with this technique is the use of an Accelerated approach to cross linking, which can shorten the treatment time from 1 hour to 30 minutes, thereby greatly increasing patient comfort.
Layers of the Cornea
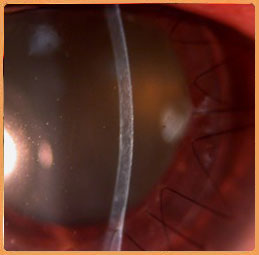
Mooren’s Ulcer
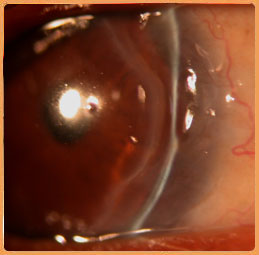
Mooren’s after surgery
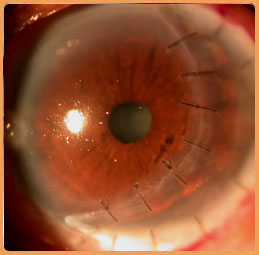
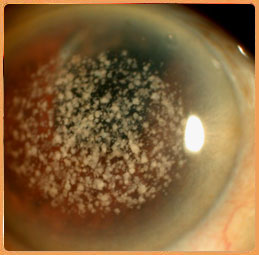
Corneal Dystrophy
After surgery day1
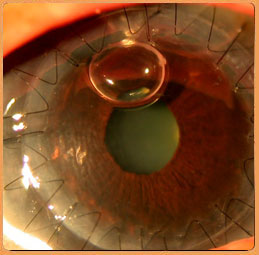
No loss in corneal clarity